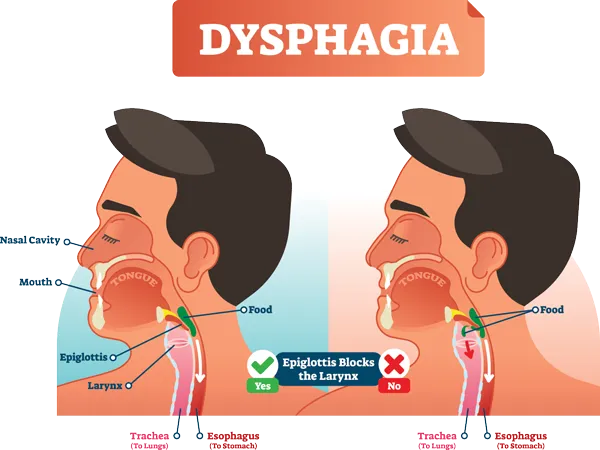
What is Dysphagia?
Dysphagia is a general term used to describe difficulty swallowing.
While swallowing may seem very involuntary and basic, it’s actually a rather complex process involving many different muscles and nerves.
Swallowing happens in 3 different phases:
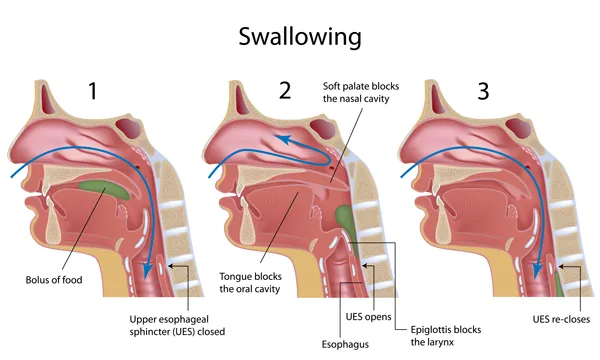
- During the first phase or oral phase the tongue moves food around in your mouth. Chewing breaks food down into smaller pieces, and saliva moistens food particles and starts to chemically break down our food.
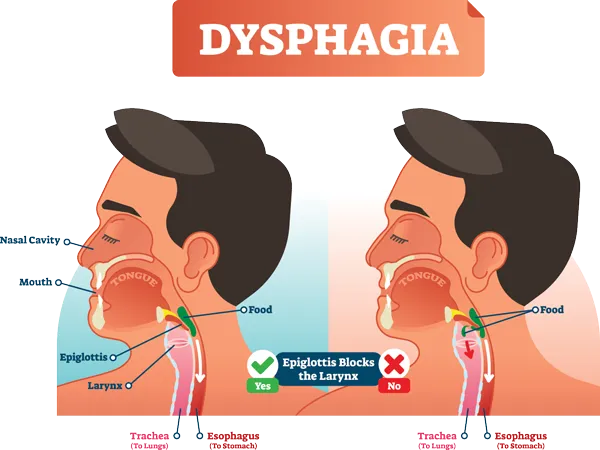
- During the pharyngeal phase your tongue pushes solids and liquids to the back of your mouth. This triggers a swallowing reflex that passes food through your throat (or pharynx). Your pharynx is the part of your throat behind your mouth and nasal cavity, it’s above your esophagus and larynx (or voice box). During this reflex, your larynx closes off so that food doesn’t get into your airways and lungs.
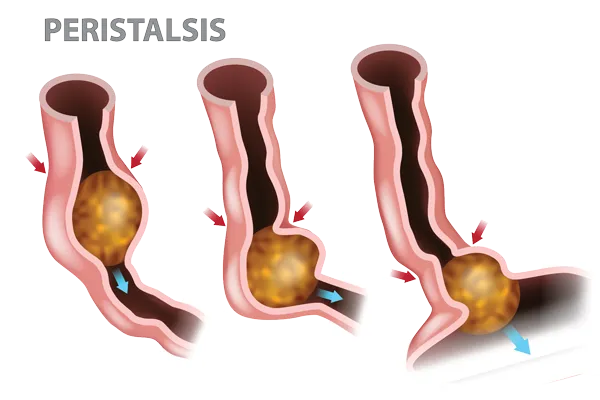
- During the esophageal phase solids and liquids enter the esophagus, the muscular tube that carries food to your stomach via a series of wave-like muscular contractions called peristalsis.
When the muscles and nerves that control swallowing don’t function properly or something is blocking your throat or esophagus, difficulty swallowing can occur
There are varying degrees of Dysphagia and not everyone will describe the same symptoms. Your symptoms will depend on your specific condition. Some people will experience difficulty swallowing only solids, or only dry solids like breads, while others will have problems swallowing both solids and liquids. Still others won’t be able to swallow anything at all.
What causes Dysphagia?
When the muscles and nerves that control swallowing don’t function properly or something is blocking your throat or esophagus (like an esophageal tumor, severe inflammation in your esophagus, or a thyroid goiter), difficulty swallowing can occur.
What are the different types of Dysphagia?
Dysphagia is often described based on where the problem originates. If it involves your mouth or throat (pharynx), it’s known as Oropharyngeal Dysphagia. If it involves your esophagus, it’s known as Esophageal Dysphagia.
Causes of Oropharyngeal Dysphagia include:
- Neurologic disorders like Multiple Sclerosis, Muscular Dystrophy, ALS, Parkinson's disease, and Huntington’s chorea.
- Stroke, brain or spinal cord injury, trauma, or surgery.
- Cancers of the head and neck
- Certain cancer treatments like radiation to the head or neck
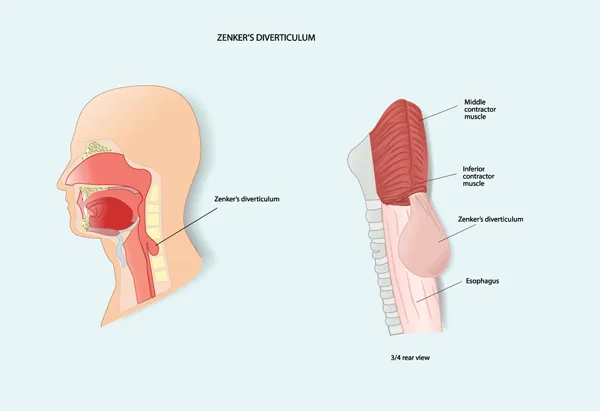
- Zenker's diverticulum (or hypopharyngeal diverticulum). This is when a pouch forms at lower part of your throat where your throat meets your esophagus. It usually happens due to tightness in the cricopharyngeus muscle. This muscle normally relaxes during swallowing. When it doesn’t, over time, pressure builds up in your lower throat and the bulge or diverticulum develops. It’s more common with age and certain neurologic conditions. Food particles can collect in this pouch causing difficulty swallowing, coughing up regurgitated or undigested food particles shortly after eating, bad breath, and recurrent throat clearing. Surgical repair may be necessary.
- Other conditions that cause strictures or narrowing of the oropharynx.
Causes of Esophageal Dysphagia include:
- Esophageal strictures. This is a narrowing in your esophagus. Tumors or scar tissue can cause the esophagus to narrow and strictures to form. Individuals who have longstanding esophagitis due to chronic acid exposure seen in GERD, or repetitive exposures to food or environmental allergens seen in eosinophillic esophagitis can develop strictures. Long-term aspirin and NSAID medications are harsh on the esophagus and can be associated with stricture formation. Other risk factors include peptic ulcer disease, alcohol abuse, and hiatal hernia. All of these conditions can irritate the lining of the esophagus, leading to scar tissue and stricture formation.
- Esophageal rings or webs are thin folds of tissue that form in the esophagus and narrow the esophagus. Some esophageal webs are inherited. Others are thought to be associated with certain autoimmune diseases and iron deficiency anemia.
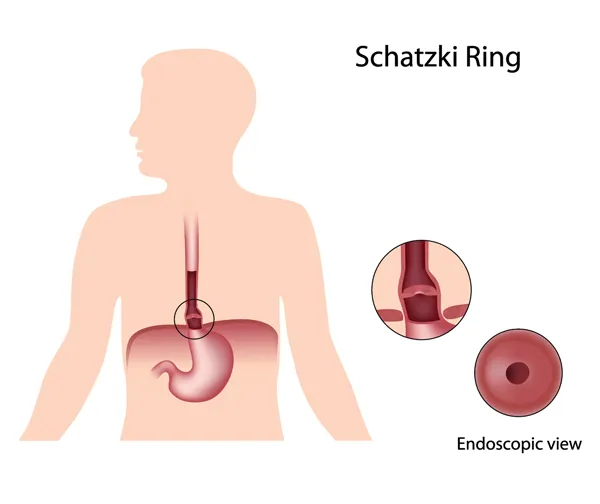
- Schatzki’s ring is a narrowing of the lower esophagus caused by changes in the lining of the esophagus. It’s associated with hiatal hernias and longstanding untreated GERD. Chronic acid exposure causes inflammation and damage to the lower esophagus leading to scar tissue formation and the formation of the Schatzki’s ring. The bigger your ring, or the more narrowing it creates, the more likely you are to have symptoms. Symptoms may include the sensation that food in stuck in your throat or chest, severe chest pain, and intermittent trouble swallowing. Complications can include blockage of the esophagus and food impaction requiring surgical intervention. Treatment options include balloon dilation during endoscopy
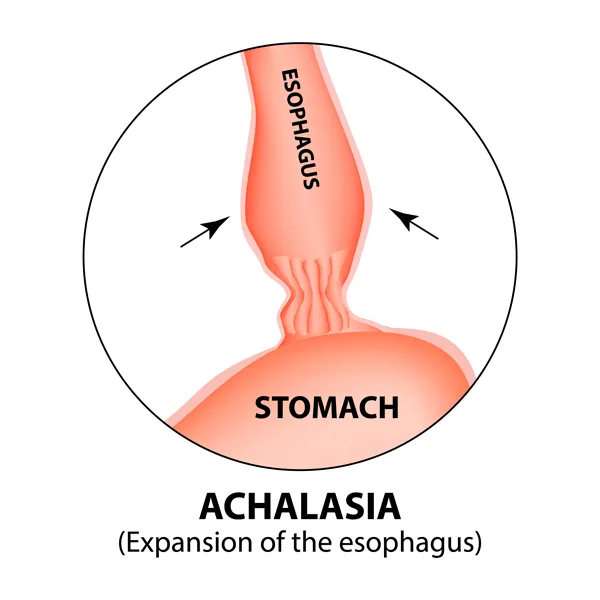
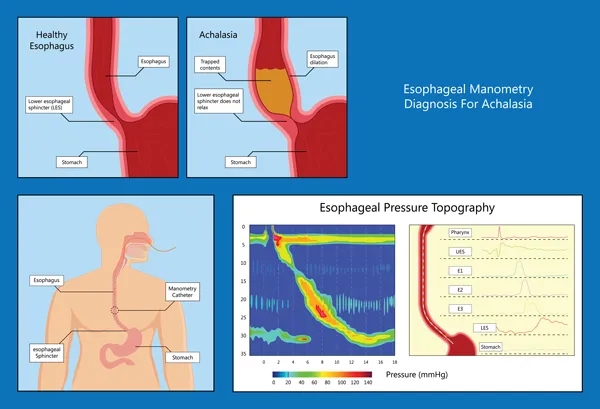
- Achalasia means failure to relax. When your lower esophageal sphincter (or LES) fails to relax properly it allows food to come back up into your esophagus. The cause of this condition is not well understood but is believed to be due to a loss of nerve cells in the esophagus.
- Distal esophageal spasm is a condition that causes uncoordinated contractions of the muscles in your esophagus. It causes sudden and significant chest pain. The cause is unclear but it may be related to the nerves that control the muscles of your esophagus not functioning properly. Symptoms can mimic cardiac disease so cardiac and other life-threatening conditions should always be ruled out.
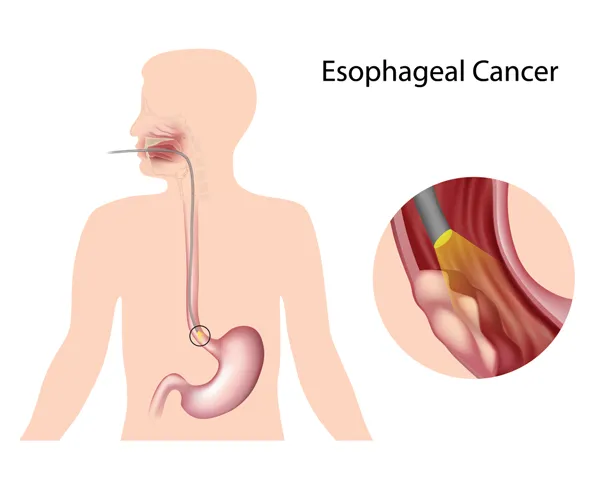
- Esophageal tumors can enlarge and block food from traveling through the esophagus. Esophageal tumors may be malignant (cancerous) or benign. Benign tumors are rare and include Leiomyomas.
- Foreign bodies like dentures can sometimes partially block off your throat or esophagus resulting in difficulty swallowing. This is more commonly seen in elderly individuals with other comorbidities, neurological disorders, or dementia
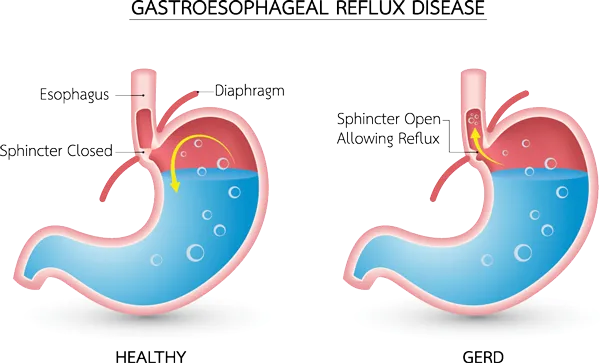
- Gastroesophageal Reflux Disease (or GERD): This is a chronic condition where acid from your stomach refluxes back up into your esophagus and causes damage to the lining of your esophagus. Causes may include: dysfunction of the lower esophageal sphincter (or LES), delayed gastric emptying, and large sliding hiatal hernias. When stomach acid chronically backs up into your esophagus this can lead to scarring and narrowing of your lower esophagus making it harder for food to pass.
- Eosinophilic esophagitis. This condition is caused by too many eosinophils in your esophagus. Eosinophils are white blood cells that help the immune system respond to allergens. The condition may be related to food or environmental allergies. It causes chronic inflammation in your esophagus, which can lead to strictures and difficulty swallowing if left untreated.
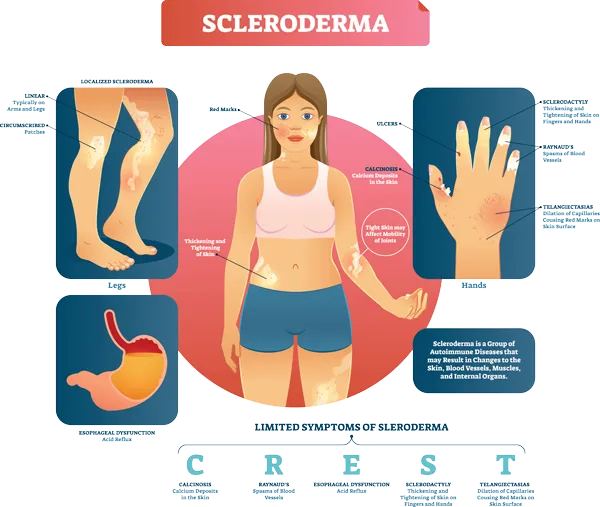
- Scleroderma is a chronic autoimmune disease that involves hardening or tightening of your skin and connective tissues. It can lead to narrowing and strictures in the esophagus, tightening of the tissue, and problems with how the muscles of the esophagus contract and relax.
- Radiation therapy can lead to inflammation and scarring of the esophagus and surrounding tissues, which can make it harder for food to pass.
- Tumors or masses from outside the esophagus can also cause problems with swallowing. For example, a very large thyroid goiter can press on the esophagus and cause symptoms of Dysphagia.
What are the Symptoms of Dysphagia?
Symptoms may include:
- The sensation that food or water is stuck in your neck, throat, or chest
- Pain with swallowing
- Being unable to swallow
- Difficulty initiating swallowing
- Drooling or slobbering
- Bringing up undigested food particles back into your mouth or nose (regurgitation)
- Heartburn or an acid taste in the back of your throat
- Coughing, choking, or gagging when swallowing
- Repeated throat clearing
- Having bad breath
- Having a consistently hoarse voice, or noticing changes in your voice
- Needing to cut foods into smaller pieces, or having to avoid certain foods because of difficulty swallowing, pain, or choking.
- Weight loss, either explained or unexplained, or as a result of not being able to consume enough calories due to difficulty swallowing
How is Dysphagia Diagnosed?
A number of different specialists might play a role in formulating your diagnosis. From a GI perspective we will often use:
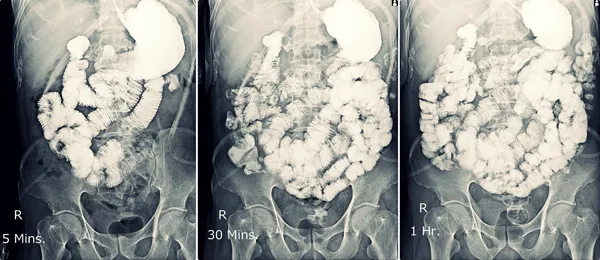
- X-rays to provide pictures of your upper GI anatomy. These x-rays might include:
- A barium swallow
- Esophogram, or
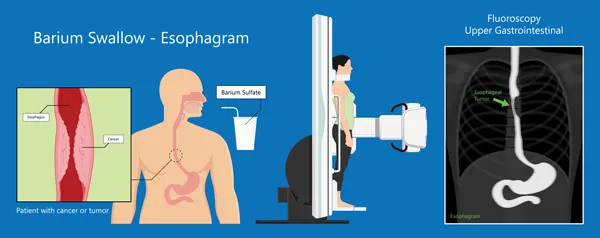
- Upper GI
- A barium swallow
- Upper endoscopy or EGD with biopsy may be used to look for reflux, GERD, strictures, webs, masses, inflammation, and other conditions such as eosinophillic esophagitis and peptic ulcer disease.
- Manometry studies are used to assess the pressure in your esophagus when you swallow and determine if your swallowing mechanisms are working properly.
- 24-hour pH impedance testing is used to determine how often acid from your stomach is getting back up into your esophagus and if your symptoms correlate with the acid levels measured during the test.
How is Dysphagia Treated?
Treatment is dependent on the specific cause of your symptoms but may include:
- Exercises for your swallowing muscles.
- Dietary modifications
- Avoidance of food allergens
- Speech therapy
- Endoscopic dilation to carefully expand any narrowed areas of your esophagus.
- Surgery, and
- Medications to treat conditions like GERD or Peptic Ulcer Disease
What are the Complications of Dysphagia?
Complications might include:
- Food Impaction where food gets stuck in your esophagus and requires regurgitation or surgical removal.
- Aspiration pneumonia. This happens when the larynx doesn’t close off properly and food or liquid enters your airways during swallowing, or when it’s regurgitated or refluxed back up into your throat and aspirated. Food can introduce bacteria into your lungs resulting in pneumonia and severe damage to your lung tissue.
- Malnutrition due to an inability to consume enough nutrients and calories
- Weight Loss
- Dehydration
- Choking and death.
- The complications of Dysphagia are very serious and can be life-threatening.
*If you are suffering from symptoms of Dysphagia please consult our office for a comprehensive medical evaluation, or if you’re experiencing emergent symptoms call 911 or go to your nearest emergency department for emergent care.
