Understanding Polyps and Their Treatment
What are Colon Polyps?
Colon polyps are small clusters of cells that grow along the lining of the rectum or the large intestine, also called the colon. Some polyps grow flat along the colon’s lining; others grow on a stalk and have a mushroom-type appearance. Most of these growths are benign and present no great cause for alarm, but the risk of developing colon cancer increases with the growth of a polyp, which can range in diameter from less than one-quarter inch to several inches.
Types of Colon Polyps
There are two common types of colon polyps: hyperplastic and adenoma. Hyperplastic polyps begin and remain benign; this type does not become cancerous. However, while not all adenomatous polyps become cancerous, all colon cancers are believed to originate with an adenoma. The likelihood of an adenoma containing cancerous cells increases with the size of the polyp. Doctors cannot identify the type of polyp without a microscope, so they strongly recommend the removal of all polyps found during an examination.
Risk Factors of Polyps

The largest risk associated with polyps is the potential for a benign polyp to grow cancerous. The risk of malignancy grows with the size of the polyp, so early detection and removal remains a person’s best means of avoiding colon cancer.
Sometimes, a large polyp partially obstructs the bowel and causes pain, vomiting, nausea and severe constipation. Removal of the polyp eliminates the symptoms.
Causes of Polyps
The exact cause of colon polyps is unknown despite their common occurrence, but certain factors are known to increase the probability of polyp development.
- Age: Age doesn’t cause polyps, but colon polyps occur most often in people over the age of 50.
- Family and Personal History: A family history of polyps increases the risk factor in individuals, and individuals who have previously developed the growths have an increased chance of recurrent growths.
- Alcohol and Tobacco Use: Smoking and excessive drinking, especially of beer, contributes to colon polyps’ development.
- Diet: Polyp formation occurs more frequently in people following high-fat, low-fiber diets than in those following low-fat, high-fiber diets.
Symptoms of Polyps
People with colon polyps often experience no symptoms and remain unaware of the growths’ presence until a doctor’s examination. Occasionally, however, diarrhea, narrow stool, bloody stool, rectal bleeding and partial bowel obstruction accompany polyps.
Finding Polyps
Doctors employ several techniques to screen patients for polyps.
Colonoscopy
Doctors use a slender, flexible tube with a miniscule video camera to examine the rectum and entire colon. This method has preference for two reasons: It most accurately discovers polyps, and doctors can remove polyps while they examine.
Computerized Tomographic Colonography
In CTCs, computer imaging provides an extremely sensitive colon X-ray, and the doctor has the ability to rotate the image for a complete and thorough view of the entire colon and rectum.
Fecal Blood Test
Testing feces for blood lacks the accuracy of other tests, so this test often pairs with other screening methods. Because few polyps bleed, fecal blood testing often results in a false negative; additionally, blood on feces is indicative of numerous other conditions, and the test exposes only the presence of fecal blood. It doesn’t expose the cause.
Please discuss other screening methods with your gastroenterologist.
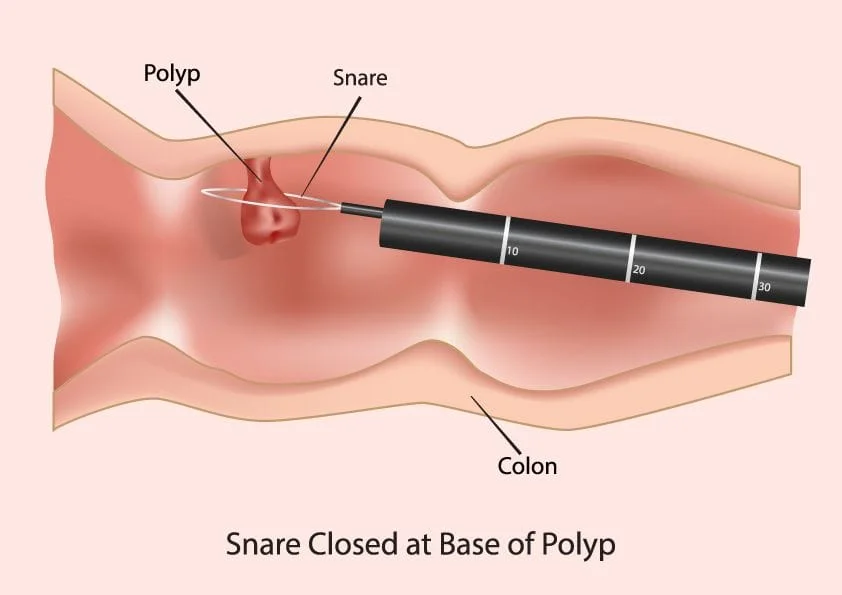
Removing Polyps
Doctors remove the majority of polyps during a colonoscopy using a snare technique: They use a wire loop that cuts and cauterizes. For smaller growths, an electric current can be used to burn the polyp. Although some growths require invasive surgery, the less invasive laparoscopic surgery generally suffices for large or inaccessible polyps that can’t be removed during a colonoscopy.
Risk of Removal
Although rather uncommon, polyps’ removal can result in bleeding or colon perforation. Simple cauterization corrects bleeding, but surgery might be required to fix perforations.
Follow-Up Colonoscopies
The frequency of follow-up colonoscopies varies according various factors that include the type, size and number of previous polyps and how well a doctor can see the colon’s surface; clear viewing of the colon depends upon the quality of the colon cleanse prior to the procedure.
Generally, a follow-up colonoscopy is recommended after five years if no subsequent polyps are found, within three to five years after the discovery of small polyps and, possibly, within months if large, flat polyps are found. However, individual follow up regimens must be confirmed with the doctor who performed the colonoscopy.
DISCLAIMER: PLEASE READ CAREFULLYThe information on this website is to provide general guidance. In no way does any of the information provided reflect definitive medical advice and self diagnoses should not be made based on information obtained online. It is important to consult a best in class gastroenterologist regarding ANY and ALL symptoms or signs as it may a sign of a serious illness or condition. A thorough consultation and examination should ALWAYS be performed for an accurate diagnosis and treatment plan. Be sure to call a physician or call our office today and schedule a consultation.
