
What are Functional Gastrointestinal Disorders?
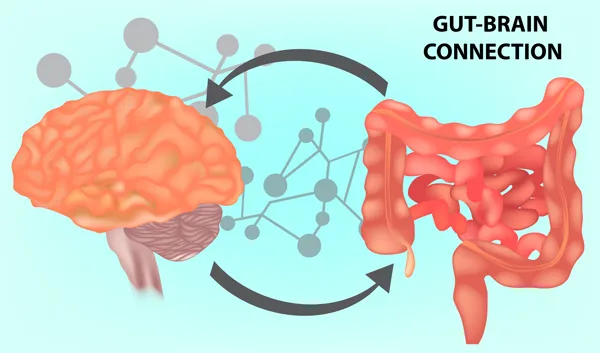
These are a group of disorders that affect how the gut and brain interact together.
These disorders don’t cause any structural, anatomical, or biochemical abnormalities. Routine medical tests used to diagnose GI disorders, like colonoscopy, upper endoscopy (EGD), abdominal ultrasound, CT or MRI, and blood and stool studies are almost always normal. Yet, the GI tract is not functioning normally. Intestinal motility can be disturbed, the sensitivity of the nerves of the intestinal tract to stimuli can be heightened, gut flora can be altered, immune function and mucosal function can be altered, and the way the brain controls some of these functions can be impaired. With these disorders there is a problem with how the gut and brain interact.
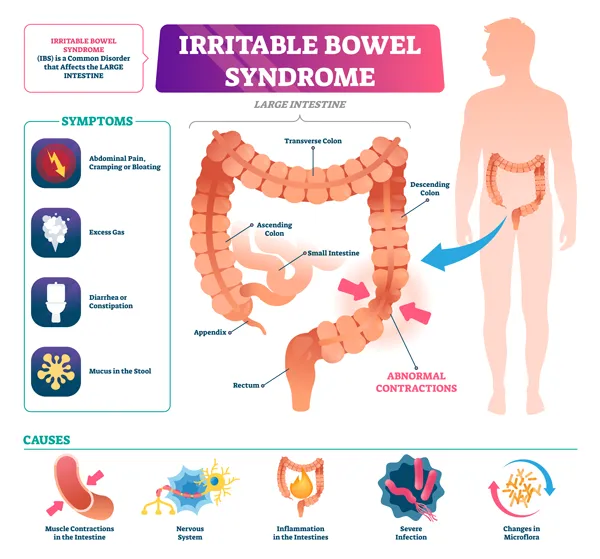
Examples of Functional Gastrointestinal Disorders include:
- Irritable Bowel Syndrome (IBS), IBS-C, and ISB-D
- Functional dyspepsia or indigestion (a term to describe symptoms of stomach pain or discomfort, nausea, bloating and belching not caused by an ulcer or other conditions),
- Functional vomiting (a term to describe recurrent unexplained vomiting at least once a week that’s not cyclical or explained by another condition),
- Functional abdominal pain (or pain without an identifiable cause), and
- Functional constipation or diarrhea (constipation or diarrhea that doesn’t meet the criteria for IBS and lacks a structural, anatomical, or biochemical cause).
While there might not be any objective findings to explain Functional Gastrointestinal Disorders, these conditions are very real, and symptoms can significantly affect your quality of life.
What Causes Functional Gastrointestinal Disorders?
Functional Gastrointestinal Disorders occur due to a problem with how the gut and brain interact, resulting in problems with GI motility, GI sensation, and other gut-brain connections.
- GI motility refers to how food is transported through the digestive tract. Normally, food is pushed through the digestive tract via peristalsis or the involuntary contraction and relaxation of muscles of the GI tract.
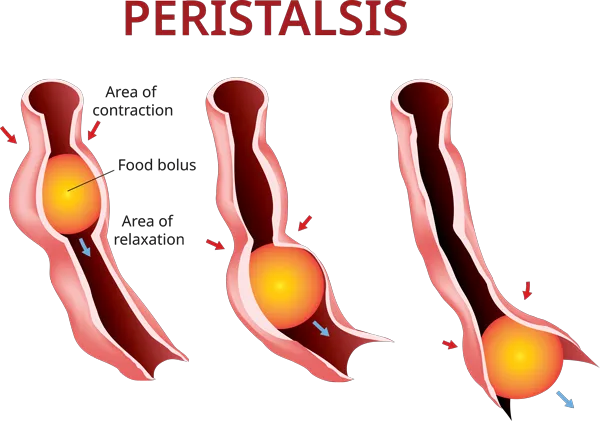
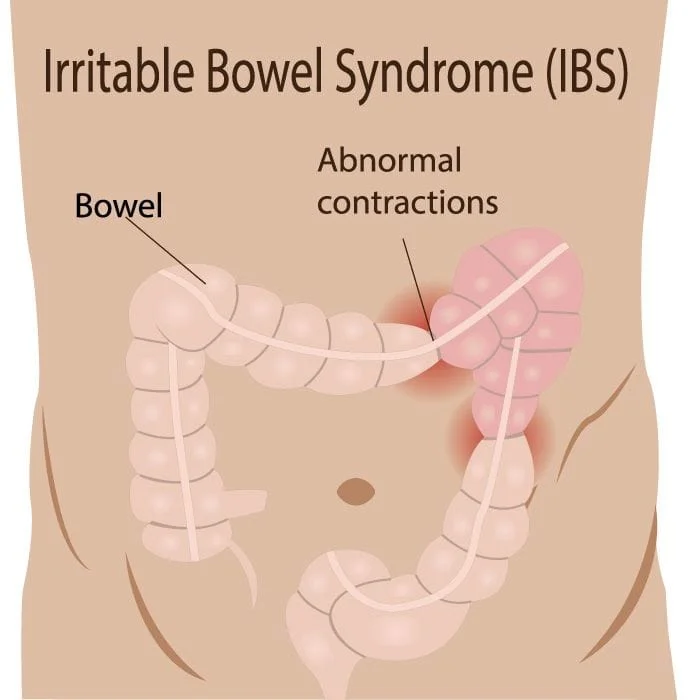
In Functional GI disorders your intestinal muscles don’t contract or relax properly. Rapid contractions cause stool to move through the digestive tract too fast resulting in loose and watery stools. Slow or weak contractions cause constipation. These abnormal contractions or spasms can cause abdominal pain and discomfort as well.
- GI sensation refers to how the nerves of the GI tract respond to stimuli like food, intestinal spasms, medications, dietary changes, hormonal fluctuations, and stress. In Functional GI disorders the nerves seem to be overly sensitive. They’re more easily excited, resulting in symptoms of pain and discomfort. You might notice a heightened sense of awareness of your gut, and feel pain or discomfort from gas or intestinal muscle contractions that other people don’t feel.
- Impaired communication between the gut and brain is believed to contribute to the development of symptoms. The brain may be sending or receiving mixed messages from the gut to contract too hard or push food along too quickly, resulting in diarrhea and urgency, or not to contract hard enough, resulting in constipation, abdominal fullness and bloating. While stress and anxiety are not thought to cause IBS, external stressors, life situations, trauma, emotions, anxiety, depression, and other psychological variables can affect GI motility and sensation and play a role in the development of Functional GI disorders.
How are Functional Gastrointestinal Disorders diagnosed?
Unfortunately, there are no routine diagnosis tests available to diagnosis these conditions. Tests like colonoscopy, upper endoscopy (EGD), ultrasound, cross sectional imaging tests (CT or MRI), blood and stool studies, are almost always normal.
Diagnosis is made primarily based on symptoms. Functional Gastrointestinal Disorders are diagnoses of exclusion. When other diseases of the GI tract like celiac disease, inflammatory bowel disease, cancers, masses, and bowel obstruction have been ruled out, we rely history and physical exam findings, pertinent negative test results, and tools like the Rome criteria to help us make a proper diagnosis. Rome criteria are standards that help us classify and diagnose Functional GI disorders.
How can nutrition help to manage the symptoms of Functional Gastrointestinal Disorders?
There’s not one specific proven diet that will work for everyone. Everyone’s food triggers will be different so it often helps to keep a food and symptom diary to identify your own personal food triggers. One way to do this is through a low FODMAP diet.
FODMAP is an acronym for “Fermentable Oligo, Di, and Mono- saccharides and Polyols”, or Fermentable oligosaccharides, disaccharides, and monosaccharides and polyols. These are short chain carbohydrates and sugar alcohols that are poorly absorbed by the body. Some people with Functional Gastrointestinal Disorders find that they are more sensitive to certain FODMAPs than others.
About 50% of IBS patients will notice an improvement in their symptoms by following a strict low-FODMAP diet TEMPORARILY. The low FODMAP diet is not intended to be followed life-long! It’s merely a short-term tool used to identify personal food triggers. Once food triggers are identified, under the supervision of a nutritionist, you will slowly reintroduce foods back into your diet one at a time creating a life-long dietary plan for you that’s both manageable and minimizes your symptoms.
FODMAPs are not the cause of Functional GI Disorders. Naturally occurring FODMAPs like fiber actually help with digestion, they help to bulk the stool and prevent constipation, and may even help to lower your risk of certain cancers of the colon and rectum. FODMAPs can, though, be poorly absorbed in the intestine, they can draw extra water back into the intestines and make you feel boggy and bloated, and they are rapidly fermented by bacteria in the large intestine which can lead to excess gas and bloating. As a result, they might trigger symptoms for certain people with Functional GI Disorders. Identifying your specific food triggers will help you to create a life-long individualized dietary plan that is manageable for you and focuses on avoiding your own specific food triggers so that you can feel at your best.
This diet should only be followed under the direct supervision of a trained nutritionist.
Following a low FODMAP diet without a proper medical evaluation and diagnosis could result in serious health problems. These types of diets can mask underlying digestive symptoms or disorders that require different treatment approaches. Please contact our office first before starting any diet or treatment plan to avoid missed diagnoses, delayed care, and poor outcomes.
How does the low FODMAP Diet work?

This is an elimination diet conducted under the direct supervision of a trained nutritionist.
High FODMAP foods are eliminated from your diet completely, or drastically minimized, for 3-8 weeks, then gradually reintroduced back into your diet to identify food triggers.
This diet is not meant to be followed long-term. It is merely a short-term tool used to identify individual food triggers. Once food triggers are identified you will slowly reintroduce foods back into your diet one at a time.
Step 1. FODMAP Elimination
Here you’ll only consume foods that contain few or no FODMAPS.
Step 2. FODMAP Reintroduction
Next, you’ll identify which foods and FODMAPs trigger your symptoms. You’ll gradually reintroduce high-FODMAP foods back into your diet one at a time. If a certain food causes no symptoms, you’ll know you can include that food in your diet moving forward. If it causes symptoms, you’ll want to avoid it.
Step 3: FODMAP Integration
This is your individualized dietary plan. It’s what you’ll follow long-term to feel at your best.
Resources that might help: https://www.ibsdiets.org/fodmap-diet/fodmap-food-list/
What other lifestyle or dietary modifications might help minimize the symptoms of Functional Gastrointestinal Disorders?
First and foremost, get a proper diagnosis. Be seen by a trained medical provider. Call our office to schedule an appointment for a comprehensive medical evaluation.
Other Lifestyle and dietary modifications that might help include:
- Follow a balanced diet to promote a healthy weight and an overall feeling of health and wellbeing. Don’t overeat. Don’t eat too late at night. Be mindful of what you’re eating, slow down while you’re eating, chew your food thoroughly, and consciously think about each bite. Don’t eat while watching TV or working on your computer.
- Avoid processed foods
- Eliminate artificial sweeteners
- Minimize alcohol
- Avoid your own personal food triggers
- Consider a low FODMAP diet temporarily under the guidance of a trained nutritionist or dietician to identify these food triggers
- Avoid foods known to cause excess gas including: cabbage, broccoli, cauliflower, onions, celery, carrots, dried beans, peas, other legumes, lentils, prunes, carbonated beverages, and raw fruit
- Reduce stress
- Get enough sleep
- Participate in regular exercise. Exercise helps by improving an overall sense of wellbeing. It helps to keep your digestive tract working properly, and potentially improves constipation. Always talk with your doctor first before beginning any exercise routine.
- Maintain an active lifestyle
- Balance your gut flora. Talk to our office about whether probiotics or natural sources of probiotics like yogurt, sauerkraut, some soft cheeses, kefir, tempeh, sour pickles, and sour dough bread might be beneficial for you.
- Make sure you’re consuming enough fiber in your diet
- Follow good bowel habits. Don’t hold it. Avoid constipation.
- Drink plenty of water. Stay hydrated.
- Drink plenty of water. Stay hydrated.
- Quit smoking
