
What is menopause?
Menopause is the stage in life when a woman’s menstrual cycle permanently ends, and she no longer has her menstrual period for at least 1 year (or 12 months). Menopause occurs when the ovaries stop producing high levels of estrogen and progesterone, and stop releasing eggs.
Peri-menopause is the stage that leads up to menopause and can start anywhere from 8-10 years prior to menopause. Post-menopause is the stage after menopause.
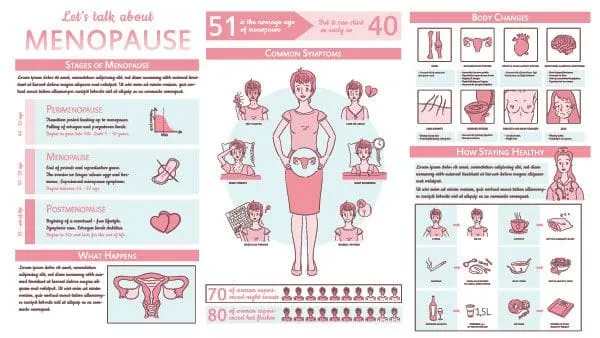
Menopause results in many changes in a woman’s body and metabolic health.
- Before menopause, women have a lower risk of heart disease associated with obesity compared to men. The sex hormones, estrogen and progesterone, have been proposed to play a protective role in the development of this type of cardiovascular disease.
- Menopause is also associated with a change in the way our bodies distribute fat. Women may notice an increased tendency toward central fat distribution around the waist with menopause. Central obesity and increased waist circumference are associated with an increased risk of cardiovascular disease and metabolic syndrome.
- The liver plays an important role in fatty acid, triglyceride, and cholesterol metabolism. Estrogen acts on the liver to reduce total cholesterol in the body by increasing good cholesterol (HDL) and decreasing bad cholesterol (LDL). Menopause is associated with an increase in bad cholesterol (or LDL), a decrease in good cholesterol (or HDL), and an increase in triglycerides (or fats). Elevated cholesterol and dyslipidemia increases one’s risk for cardiovascular disease.
- Estrogen also influences how our body uses calcium.
- Considering these variable and more, post-menopausal women are at increased risk for metabolic syndrome, high cholesterol, increased glucose and insulin levels, diabetes, cardiovascular disease, and osteoporosis.
Estrogen and progesterone affect many of our organ systems and metabolic processes. The digestive tract is not excluded! As a result, peri-menopausal and postmenopausal women often have a high prevalence of GI symptoms and complaints associated with fluctuating hormone levels.
- Fluctuations in estrogen and progesterone levels around the time of menopause will often trigger IBS symptoms in women and may exacerbate underlying GI disease.
- Alterations in progesterone and estrogen levels related to menopause can affect how fast food moves through the GI tract, and symptoms of constipation.
- Higher levels of estrogen and progesterone, especially during peri-menopause, may slow your intestinal movements and cause constipation.
- As well, certain conditions like diabetes and metabolic syndrome that become more common with menopause increase a woman’s risk for developing certain GI conditions. For example, the most common cause of gastroparesis (or delayed stomach emptying) is diabetes.
- Estrogen tends to be somewhat protective against Barrett’s esophagus until the protective effects of estrogen wear off with menopause. After menopause, women and men show SIMILAR rates of Barrett’s esophagus. Barrett’s esophagus affects BOTH men and women!!!
- Constipation tends to worsen with age, and can be associated with other endocrinopathies that are often more common in females AND with age like hypothyroidism. As such, a lot of symptoms and disease states can arise with the onset of menopause.
What GI symptoms are associated with menopause, and WHY?

A wide range of digestive problems can arise during menopause including excessive gas, bloating, belching, nausea, and abdominal discomfort.
If you think about it, the main job of our digestive tract is to break down food, absorb nutrients, and excrete waste. Hormones play a large role in digestion. When estrogen and progesterone levels change during, and leading up to, menopause, this can alter the entire process of digestion.
Estrogen plays a key role in keeping our cortisol levels low. Cortisol is our primary stress hormone. Its job is to make sure you’re able to respond appropriately to both good and bad stressors. Corisol increases sugar (or glucose) in your bloodstream so that you have energy available to react to a stressful situation. It enhances your brain's ability to use glucose so that you can respond more efficiently to stress and think more clearly under pressure. It slows or halts body functions that wouldn’t be essential in a fight-or-flight situation. For example, it suppresses your GI tract and reproductive systems in a time of stress: organ systems that aren’t essential when you just need to survive
That being said, when estrogen levels decline in menopause, cortisol levels rise. This can have several effects on the GI tract including reduced production of stomach acid (or HCL), and slowed GI motility. “Slowed GI motility” means it takes longer for food to travel through your digestive tract. This results in gas, bloating and constipation.
Too little progesterone can also slow GI motility. The longer food remains in your colon, the more water is reabsorbed from your stool back into your bloodstream, and the harder and drier your stools get. Constipation ensues.
Apart from menopause, as we age our GI tract naturally slows down adding to these symptoms of gas, bloating and constipation.
How does menopause affect CONSTIPATION?
There is a direct link between hormonal changes and bowel activity. Declining levels of estrogen and progesterone associated with menopause slow GI motility, meaning it takes longer for food to get through your GI tract. The longer food remains in your colon, the more water is reabsorbed back into your bloodstream, and the harder your stools get.
Additionally, during peri-menopause and menopause, lower estrogen levels decrease bile levels. Bile is produced by the liver and stored in the gallbladder. It mixes with fats and helps to dissolve and absorb them. Bile salts help to promote bowel movements by softening stool, lubricating your intestines, and speeding up how fast stool moves through your colon. Decreased bile levels associated with menopause can make stools harder and more difficult to pass resulting in constipation, gas and bloating.
Constipation related to menopause may also be exacerbated due to weakened pelvic floor muscles. Your risk for pelvic floor weakness and pelvic floor dysfunction increases with age.
Finally, hypothyroidism and diabetes are more common as we age and with menopause. These conditions can contribute to and exacerbate constipation.
Often post-menopausal women will have multiple risk factors for constipation. Addressing all of these issues thoroughly and comprehensively will help you to experience the best quality of life and alleviate your symptoms to the fullest extent possible.
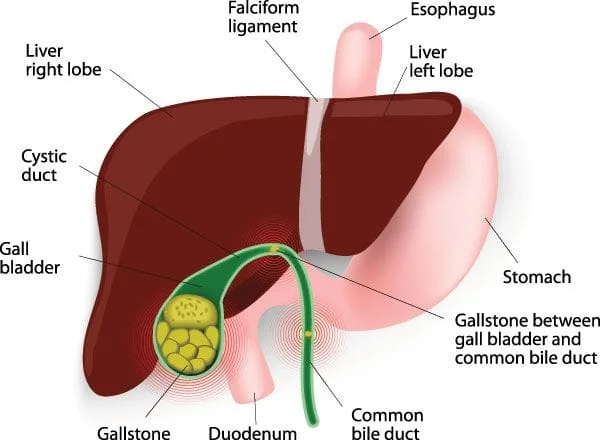
How does menopause affect Gallbladder Disease?

Female gender, increasing age, pregnancy, estrogen therapy, both long-term oral contraceptive use and hormone replacement therapy, are all risk factors for gallbladder disease and gallstones.
Gallbladder disease is more common in women than men. This is because women have more estrogen and progesterone than men. Both estrogen and progesterone change the composition of bile salts, and affect how fast bile moves through the biliary tract.
The biliary tract consists of the liver, gallbladder and bile ducts. These are the organs and structures that work together to make, store, and secrete bile.
Bile helps you to digest fats. It’s made mainly of water. The bile salts in bile are what actually break down fat molecules in your small intestines into smaller droplets that your intestines can absorb more easily.
When estrogen and progesterone levels drop in menopause, blood cholesterol levels increase, bile takes on a higher concentration of cholesterol, the gallbladder doesn’t empty as quickly as it did before, bile sits in the gallbladder stagnant for longer periods of time, and gallstones and gallbladder disease are more likely to develop.
How does menopause affect BLOATING?
When women reach peri-menopause, estrogen levels can actually fluctuate quite a bit, at least initially. They tend to rise and fall before dropping off significantly at menopause. When estrogen levels are high women tend to retain more water. Bloating results.
During and after menopause, bloating can be related to slowed digestion and constipation related to hormonal imbalances.
Lower estrogen levels result in decreased levels of bile. Bile promotes bowel movements by softening your stool, lubricating your intestines, and speeding up how fast stool moves through your large intestine. Decreased bile levels associated with menopause can make stools harder and drier and more difficult to pass resulting in constipation, gas and bloating.
In order to avoid missed diagnoses, delayed care and poor outcomes ALL GI symptoms should always be evaluated promptly and aggressively by a trained gastroenterologist. Bloating can be a sign of a much more serious problem like certain cancers, ovarian cancer, pancreatic cancer, liver disease, inflammatory bowel disease, bowel obstruction, diverticulitis, infectious causes, amongst many other conditions.
How are Diarrhea and Incontinence related to menopause?

When progesterone levels decrease associated with menopause you may experience an increase in your bowel activity meaning food may move through your GI tract more quickly resulting in diarrhea, increased gas, and bloating.
Post-menopausal women may be more inclined to experience incontinence, diarrhea, and constipation due to pelvic floor dysfunction, and a weakened pelvic floor. Your pelvic floor, or the muscles, ligaments, connective tissues, and nerves that support the bladder, uterus, cervix, vagina, and rectum, and hold these structures in place and help them to function, plays an important role in bowel movements.
Your pelvic floor muscles stretch from your tailbone in the back to your pubic bone up front, and from one hip to the other side to side. They move up and down like a trampoline supporting your internal organs.
Normally, when you go to the bathroom your body tightens and relaxes its pelvic floor muscles in a coordinated fashion. When you have pelvic floor dysfunction, your body keeps tightening these muscles instead of relaxing them when it should.
Women are at increased risk for a weakened pelvic floor as a result of pregnancy and childbirth. Pelvic Floor Dysfunction is also more common with age. Properly diagnosing and treating pelvic floor dysfunction is crucial to managing symptoms of diarrhea, constipation and incontinence in affected patients.
How is IBS affected by Menopause?
Symptoms of IBS such as diarrhea, constipation, and bloating are often worsened by menopause due to the effects of estrogen and progesterone on GI motility and function. Hormonal imbalances can exacerbate underlying GI disease and make diarrhea, constipation, gas and bloating worse.
Can Menopause cause Nausea?
During peri-menopause estrogen production by the ovaries can fluctuate greatly. When estrogen production is high, women may experience nausea associated with these hormonal fluctuations.
Nonetheless, in order to avoid missed diagnoses, delayed care, and poor outcomes ALL GI symptoms should be evaluated promptly and aggressively by a trained gastroenterologist. Nausea can be a sign of a much more serious problem such as certain cancers, ovarian cancer, pancreatic cancer, liver disease, inflammatory bowel disease, bowel obstruction, and other conditions.
If you’re concerned about GI symptoms associated with menopause, please contact our office for a comprehensive medical evaluation.
*This information is only intended for educational purposes and the accuracy of this content is not guaranteed.
