What is H. pylori?
H. pylori is a spiral shaped bacterium that can cause inflammation and ulcers in the lining of your stomach and small intestine. Inflammation in your stomach is referred to as gastritis. Inflammation in your duodenum (the first part of your small intestine) is known as duodenitis. Peptic Ulcer Disease refers to painful sores or ulcers in the lining of your stomach or duodenum. It is thought that H. pylori may be responsible for up to 80% of stomach ulcers and 90% of duodenal ulcers.
What causes H. pylori infection in the GI tract?
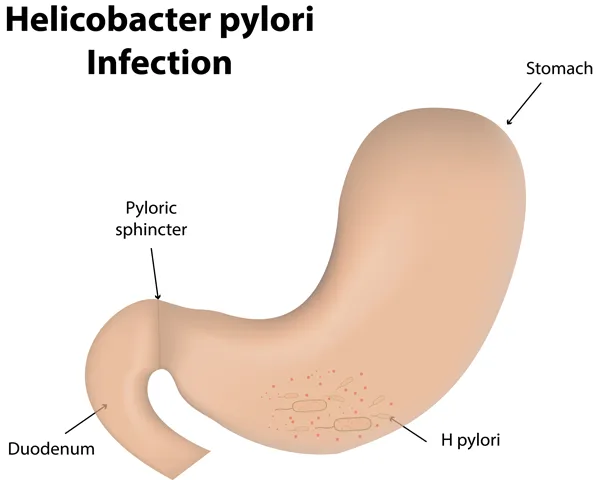
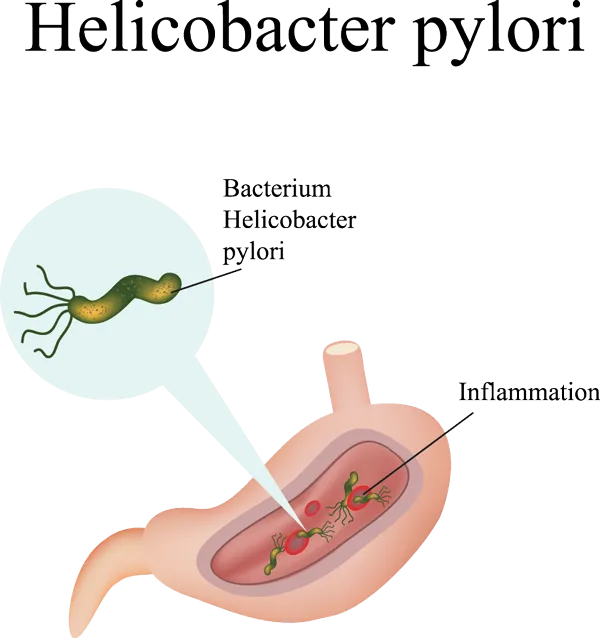
H. pylori infection is caused by a spiral-shaped, gram-negative, bacterium. The mode of transmission is not completely clear; however it may be passed from person to person through direct contact with saliva, vomit or fecal matter, through the fecal-oral, or oraloral route. It may also be spread through contaminated food or water.
How common is H. pylori?
H. pylori infection is common in the United States. About 20% of people <40 years of age, and half of people >60 years of age are infected, although not everyone will have symptoms. Most people will actually be asymptomatic.
Worldwide it affects roughly 50-60% of the adult population.
As many as 90% of people with Peptic Ulcer Disease may be infected with H. pylori.
What are the risk factors for H. pylori?
Risk factors may include:
- Smoking
- Crowded living conditions
- Consuming contaminated food or water sources
- Unsanitary water
- Living in a developing country
- Living with someone who has the infection
- Consuming restaurant food
- Consuming meat and fish
- Ethnicity: Hispanics and African Americans may be at increased risk.
- Genetics: It is not well understood why some people are colonized with H. pylori and do not develop peptic ulcer disease or GI inflammation; however, there may be a genetic component that protects some individuals and makes them more resistant to the harmful effects of the bacteria and not others.
- Small sized studies have suggested that chili peppers may be protective

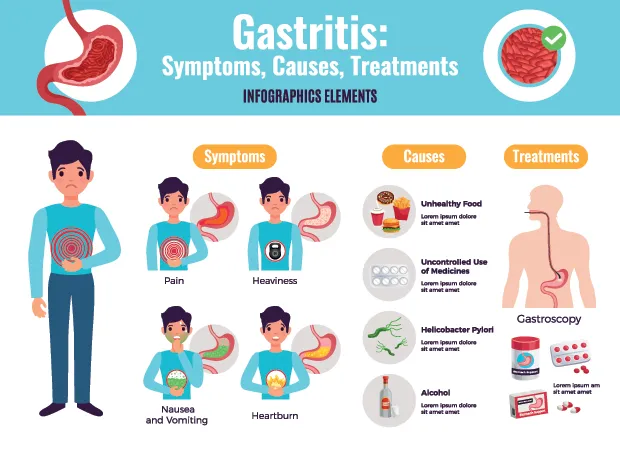
Signs or symptoms may include:
- A dull, gnawing ache in your upper middle abdomen that often comes 2-3 hours after eating or in the middle of the night when the stomach is empty.
- Abdominal discomfort or pain that's worse when your stomach is empty or after eating, usually in the upper middle abdomen
- Nausea, Vomiting, Indigestion, Heartburn
- Loss of appetite
- Feeling full sooner than usual (early satiety)
- Frequent burping or belching
- Regurgitation
- Bloating
- Unintentional weight loss
- Vomiting blood that is bright red, or looks like coffee grounds
- Dark, black, or tarry looking stools (due to bleeding ulcers)
- Fatigue, Weakness, and Shortness of breath (due to low red blood cell counts or anemia caused by bleeding ulcers)
- Diarrhea
- Bad breath
Is H. pylori contagious? How is it spread?
The exact way H. pylori is spread is not well understood. H. pylori may be passed from person to person through direct contact with saliva, vomit or fecal matter, via the fecaloral, or oral-oral route. It may also be spread through contaminated food, water, or utensils.
How is H. pylori Diagnosed?
H. pylori can be detected using blood antibody tests, urea breath tests, stool antigen tests, and endoscopic biopsies taken during EGD (Esophagogastroduodenoscopy).
EGD is often preferred because it allows us to both identify the H. pylori bacterium, and see the severity of your gastritis, duodenitis, or peptic ulcer disease, plus biopsy for other conditions that may be associated with longstanding H. pylori infection such as MALT lymphoma, and stomach cancer.
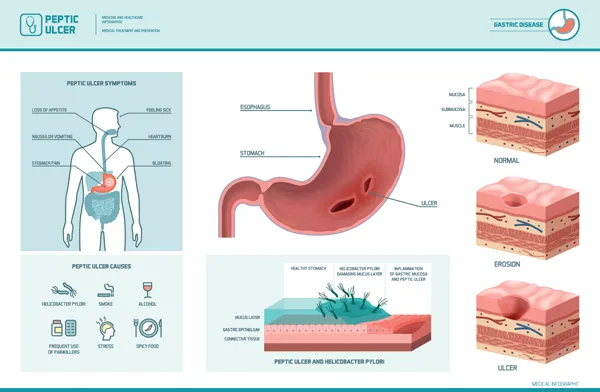
How does H. pylori cause Peptic Ulcer Disease?
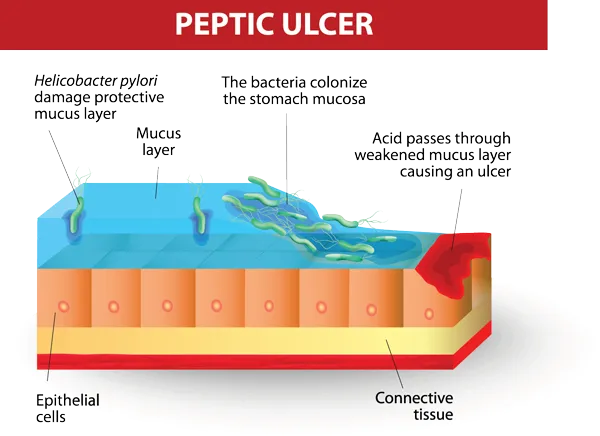
- H. pylori weakens and damages the protective mucosal lining of your stomach and small intestine, allowing acid to reach the deeper layers of these structures. Your gastric mucosa is a barrier that normally allows your stomach to safely contain acid necessary for the proper chemical digestion of food. If this protective barrier is broken down, then acid is able to penetrate through the layers of the stomach and duodenum and cause damage. Inflammation and ulcers result.
- About 10% of people with H. pylori will develop an ulcer
- As many as 90% of people with Peptic Ulcer Disease are infected with H. pylori.
- Some strains of H. pylori appear to be more prone to causing ulcers than others.
- Ulcers can bleed resulting in anemia and other life-threatening complications.
What are the complications associated with untreated H. pylori infection?
Complications associated with H. pylori infection may include:
- Inflammation of the stomach (gastritis) and duodenum (duodenitis)
- Peptic Ulcer Disease

- Anemia due to bleeding ulcers
- Bleeding ulcers
- Perforation
- MALT: People with H. pylori may be more likely to develop MALT (mucosaassociated lymphoid tissue) lymphoma.
- MALT is rare, but often quickly regresses once H. pylori is treated.
- Stomach cancer
- H. pylori may increase your risk for certain types of stomach cancer.
- Eradication seems to reduce cancer risk.
How is H. pylori Treated?
The goal of treatment is to get rid of the bacteria, to heal ulcers if they are present, and prevent the ulcers from returning.
Typically, a combination of two antibiotics and an acid-reducing medication or proton pump inhibitor (PPI) is used. This is known as triple therapy. The antibiotics kill the bacteria and the PPI helps to heal the damage caused. The drugs work together to successfully eradicate the infection. The medications are usually prescribed for 2 weeks.
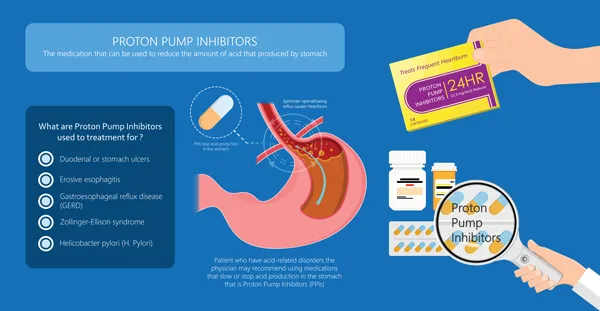
Be sure to complete your full course of treatment to reduce your risk of recurrence and to help prevent bacterial resistance.
To help ulcers heal: avoid spicy foods, highly acidic foods like tomato-based products, citrus foods, coffee and tea, avoid alcohol, manage your stress, and quit smoking!
How can I know that my treatment was effective?
We’ll confirm that your treatment was effective with a urea breath test or a stool antigen test after you complete your course of treatment. Make sure to keep all of your office visit follow-up appointments to ensure that your treatment was effective!
Follow-up EGD may be required to ensure resolution of any ulcers originally found. All ulcers should be followed to resolution to ensure that there aren’t any underlying malignancies, cancers, or other conditions masked by these finding.
What is my treatment wasn’t effective?
Patients who fail initial treatment may need to be retreated, often with a different combination of medications.
How can I prevent H. pylori?
- Practice good hygiene and frequent hand washing. Wash your hands often, and always after using the bathroom and before eating or preparing any food.
- Avoid contact with saliva, feces, or other bodily fluids of infected persons.
- Avoid contaminated or unsanitary food or water sources and utensils.
- Make sure all family members are treated if infected and a trained medical provider recommends it.
- When traveling, only drink bottled water and do not eat the skins of any fruits or vegetables.
- Properly prepare and thoroughly cook all foods.
- Complete all of the medications prescribed to you if you are diagnosed with H. pylori to prevent recurrence and resistance.