1. Choledocholithiasis
What is Choledocholithiasis?
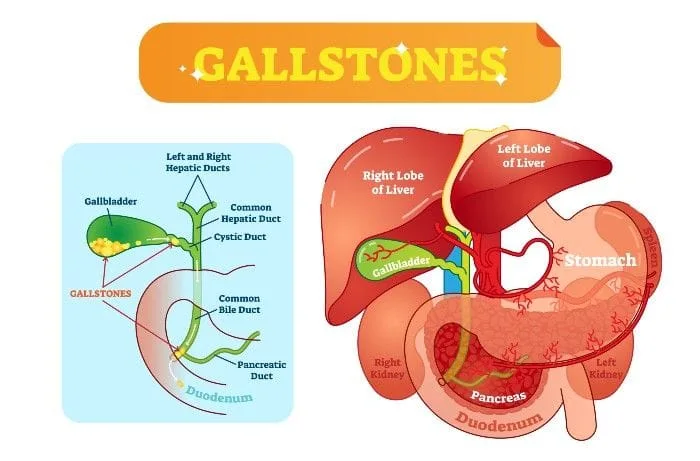
Choledocholithiasis means there are gallstones in the common bile duct. The bile duct is the small tube that carries bile from your gallbladder to your small intestine.
Gallstones usually form in your gallbladder. If they become mobile they can travel out of your gallbladder into the bile duct. They can also form separately in the bile duct.
When gallstones move out of your gallbladder they can become lodged in the bile ducts. This prevents bile from exiting the gallbladder and causes it to build up in the gallbladder and damage the lining of the gallbladder. This can lead to the gallbladder becoming inflamed or distended. If severe it can lead to jaundice, liver damage, acute pancreatitis and ascending cholangitis.
What are bile duct stones made up of?
Often they are made up of bile pigments, calcium, or cholesterol salts.
What causes Choledocholithiasis?
Stones are more likely to form if the gallbladder doesn’t empty completely or often enough. Too much cholesterol, too much bilirubin, or not enough bile salts in the bile can cause stones. The most common type of gallstones are cholesterol gallstones.
What are the symptoms of Choledocholithiasis?
Often, there are no symptoms unless the stone blocks the common bile duct. Greater than 70% of people with gallstones will be asymptomatic and their diagnosis will be made only incidentally by ultrasound performed for another reason. Roughly 10% of these people will become symptomatic within five years of diagnosis and 20% within 20 years of diagnosis.
When symptoms are present, they may include:
- Severe pain in the middle of the upper abdomen or right upper quadrant
- Fever, chills, sweats
- Nausea and/or vomiting
- Jaundice
- Pale or clay colored stools
Who is at Risk for Developing Choledocholithiasis?
One risk factor is having a history of duodenal diverticula. People with a history of gallstones or gallbladder disease are also at risk for bile duct stones. Even if you’ve had your gallbladder removed you can still experience bile duct stones.
Risk factors for gallstones in general include:
- Obesity
- Low-fiber, high-calorie, high-fat diet
- Pregnancy
- Prolonged fasting
- History of rapid weight loss
- Older adults typically have a higher risk
- Women of child-bearing age are more likely to have gallstones
- Asians, Native Americans, and Mexican Americans are at higher risk
- Genetics may play a role
How is Choledocholithiasis diagnosed?
By imaging studies such as CT scan, abdominal ultrasound, MRI. Laboratory tests including liver function tests, complete blood count, and pancreatic enzymes may help. Sometimes ERCP (Endoscopic retrograde cholangiography) or MRCP (Magnetic resonance cholangiopancreatography) are necessary.
What is the Treatment for Choledocholithiasis?
Treatment involves an operation called a choledocholithotomy, or the removal of the stone using ERCP (endoscopic retrograde cholangiography), a minimally invasive procedure that combines x-ray and upper endoscopy. Here, an endoscope, a lighted, flexible tube, is passed through the mouth and into the duodenum. Then a contrast dye is injected into the bile ducts so that they can be seen on x-ray. Special tools are guided through the endoscope to remove the stones.
Sphincterotomy during ERCP, which makes a surgical cut into the muscle in the common bile duct to allow stones to pass or be removed, is sometimes used.
The goal of treatment is to relieve the blockage.
What are the complications of Choledocholithiasis?
Stones in the bile duct can cause infection. Long-standing stones can lead to secondary biliary cirrhosis or hardening of the liver. Bile duct stones can cause jaundice, liver damage, acute pancreatitis, and a condition known as ascending cholangitis.
2. Gallstone Pancreatitis
What is Gallstone Pancreatitis?
Sometimes a gallstone can block your pancreatic duct and cause pancreatitis. This is known as gallstone pancreatitis.
Gallstones are a common cause of pancreatitis. Gallstones or bile duct stones can become mobile and travel out of the gallbladder and into the common bile duct. Here, they can block the common bile duct. Since the common bile duct and pancreatic duct both join together and release their secretions in the same spot in the small intestines, a stone in this location also blocks the pancreatic duct, which prevents pancreatic enzymes from exiting the pancreas. These pancreatic enzymes then begin to irritate and almost “digest” the cells of the pancreas, causing the inflammation associated with pancreatitis.
What is the Pancreas and what does it do?
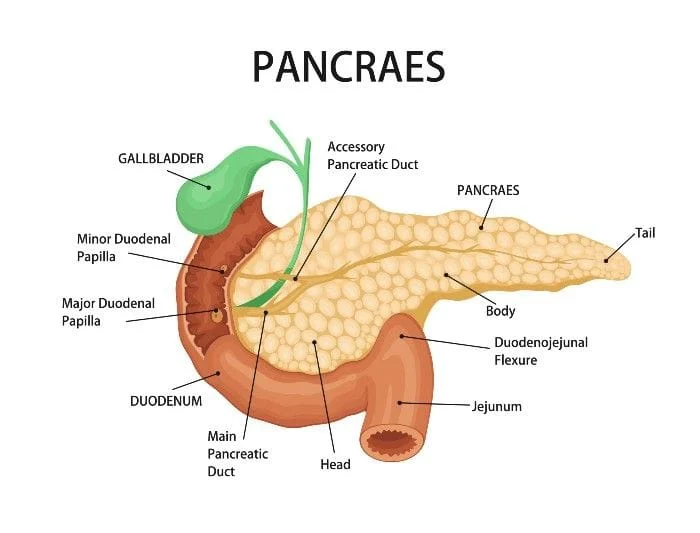
The pancreas makes fluids and enzymes that help with digestion. It really is two glands mixed together into one organ. The exocrine pancreas creates enzymes that help with digestion, and the endocrine pancreas releases hormones, like insulin and glucagon, into the blood, to help control blood sugar.
What causes gallstone pancreatitis?
Gallstone pancreatitis occurs when a gallstone blocks your pancreatic duct causing inflammation and pain in your pancreas.
The stone blocks the opening from the pancreas into the first part of your small intestine (the duodenum). This causes a backup of fluid that can travel up both the bile duct and the pancreatic duct.
What are the symptoms of gallstone pancreatitis?
Symptoms may include:
- Severe pain, particularly in the left upper abdomen
- Pain that feels sharp or a “squeezing” in your left upper abdomen or in your back
- Pain that radiates to the shoulder or chest
- Fever, chills, sweats,
- Jaundice or yellowing of the skin or eyes
- Nausea, Vomiting
How is gallstone pancreatitis diagnosed?
Gallstone pancreatitis is diagnosed via a combination of tools. Blood tests are used to measure your pancreatic enzymes, amylase and lipase, and different imaging tests such as CT, MRI, and ultrasound are commonly used to aid in the diagnosis.
How is gallstone pancreatitis treated?
Gallstone pancreatitis is usually treated with pain medications and bowel rest. Pain and nausea may need to be treated with IV medications. Surgery may be required to remove the contributing stone or stones. This is commonly done through ERCP (endoscopic retrograde cholangiography). Sometimes you may need to have your gallbladder removed.
What are possible complications of gallstone pancreatitis?
Gallstone pancreatitis can be fatal if left untreated. Serious complications include: infection, pancreatic necrosis, multiple organ failure, and death.
Digestive fluids from the liver, gallbladder, and pancreas, can back up into your body leading to severe infection. Pancreatic tissue can die, become infected, and necrose.
How can I prevent gallstone pancreatitis?
It’s not possible to fully prevent gallstone pancreatitis. This is because it’s not possible to fully prevent gallstones.
To reduce your risk of gallstones:
Follow a sensible diet, avoid crash dieting and very low calorie diets, eat plenty of fiber rich foods, like raw fruits and vegetables, beans and whole-grains, and avoid excess fat. Maintain a healthy weight. Take control of your cholesterol and metabolic health. Talk to your prescribing physician about any estrogen containing medications you might be taking.
3. Primary Sclerosing Cholangitis
What is Primary Sclerosing Cholangitis?
What causes Primary Sclerosing Cholangitis?
The cause of this condition is not well understood but approximately 60-80% of affected patients also have Ulcerative Colitis.
Many experts believe its cause is multifactorial involving the immune system and several different hepatobiliary diseases.
What are the symptoms of Primary Sclerosing Cholangitis?
Nearly half of affected patients don’t have symptoms; however, if symptoms do occur, they can include:
- Fever
- Jaundice (or yellowing of the skin and white portions of the eyes)
- Severe itching,
- Non-specific fatigue
- Upper abdominal discomfort.
- Enlargement of the liver and spleen
- Abdominal pain
- History of acute cholangitis (or infection of the bile ducts)
- Dark urine
- Malabsorption
- Fatty stools
- Cirrhosis and Portal Hypertension
How is Primary Sclerosing Cholangitis diagnosed?
Other causes must first be ruled out. Liver biopsy may be necessary. Specific clinical criteria are used to make the diagnosis based on lab, imaging, and endoscopic findings.
What is the treatment for Primary Sclerosing Cholangitis?
Supportive treatment and surveillance. Currently, the only known cure is a liver transplant. Having this condition increases your risk of liver cancer.
4. Acute Cholangitis
What is Acute Cholangitis?
Cholangitis refers to inflammation and infection of the bile duct system. The bile duct system carries bile from your liver and gallbladder to your small intestine. The condition usually happens abruptly (hence “acute”).
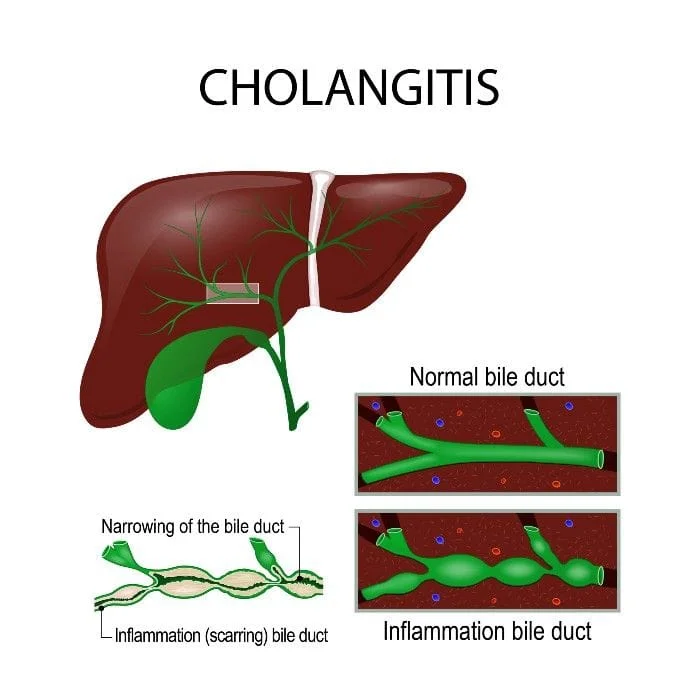
What causes Cholangitis?
In most cases cholangitis is caused by a blocked bile duct somewhere in your bile duct system. This is most commonly due to bile duct stones or sludge obstructing the bile ducts. Benign and malignant strictures can also create an obstruction. Other less common causes include:
- Tumors
- Blood clots
- Pancreatitis
- A complication of surgery
- A parasitic infection
- Primary Sclerosing Cholangitis
- And a complication of certain endoscopic procedures
What are the symptoms of cholangitis?
Individual symptoms may vary. Most patients have fever, jaundice, and right upper quadrant abdominal pain. Other symptoms may include:
- Nausea and vomiting
- Clay-colored stools
- Dark urine
- Low blood pressure
- Fatigue or lethargy
- Change in mental status
What are the risk factors for cholangitis?
- Having a history of gallstones.
- Having certain autoimmune disorders like Ulcerative Colitis or Crohn's disease
- Having had recent medical procedures involving the bile duct area
- Being immunosuppressed
- History of parasite infection or exposure
How is cholangitis diagnosed?
Based on History and Physical Exam findings, Lab tests: CBC, Liver function tests, blood cultures, and imaging studies like ultrasound, CT, and MRCP
What are the complications of Acute Cholangitis?
Acute Cholangitis can quickly become life threatening. If untreated, sepsis with shock, multi-organ failure, and death can occur.
What is the treatment for Acute Cholangitis?
Most patients require antibiotics and surgical intervention or drainage of the bile duct system.
